Learn about CO-45 in medical billing, a claim adjustment code for insurance write-offs due to contractual agreements. Discover its impact on revenue cycle management.
Healthcare professionals usually handle complex codes in medical billing, each symbolizing certain services, procedures, or reimbursement concerns. CO-45 is one of the typical codes that are frequently applied but misused at times. The code usually signifies that a claim has been corrected as per a contractual arrangement such that the provider is not able to bill the patient for the adjustment.
For a seamless medical billing experience, explore how RevMaxx can enhance efficiency and accuracy in your revenue cycle operations.
According to the American Medical Association (AMA), billing errors contribute to over $935 million in improper payments annually. Misinterpretations about CO-45 will result in billing errors and confusion. Claims in some instances are labeled as exploratory, investigative, or incorrect, leading to payment delays.
This article will describe CO-45 in medical billing, its effect, and ways to reduce errors to make reimbursement go smoothly.
CO-45 in Medical Billing
Medical billing can get complex with numerous codes, rules, and policies to abide by. A significant code is CO-45 that applies when an insurance provider denies payment for a medical service or procedure. This is typically the case when the care is deemed experimental or investigational, i.e., not proven or widely practiced in medicine. Familiarizing oneself with CO-45 can prevent billing complications and additional expenses for healthcare providers and patients.
Role of CO-45 Code
Medical billing may be complex since it has various codes, policies, and rules. Among them is CO-45, which is utilized in case a claim should be corrected and resubmitted to Medicare.
CO-45 is a medical billing code to indicate a claim is being resubmitted in its corrected form. If a claim is denied by Medicare due to errors—such as faulty patient information or improper diagnosis codes—the practitioner can correct the errors and resubmit the claim with the CO-45 code. This allows for the correct claim to be processed correctly and payment adjustments as required to be made.
When to Use CO-45
- When a claim is denied because of errors in the initial submission.
- When re-submitting a corrected claim to Medicare.
- To correct errors like patient data or code of diagnosis.
When NOT to Use CO-45
- For initial claim submissions.
- When more documents or information are needed.
Applying the CO-45 code appropriately is crucial to seamless and correct medical billing. Knowing when and how to apply it prevents delays and ensures proper processing of claims.
Implications of CO-45
Using the CO-45 code helps ensure that corrected claims are processed properly and any needed payment adjustments are made. This code should only be used for replacement claims that fix errors or missing information in the original claim. It’s important to apply it correctly to avoid issues
Correcting Errors
The CO-45 code is used when there are mistakes in the original claim, such as incorrect patient details, diagnoses, procedures, or billing codes. It allows providers to fix these errors and resubmit the claim, ensuring it is processed correctly.
Submitting a Replacement Claim
When submitting a replacement claim with the CO-45 code, providers must include the correct HCPCS codes to describe the services given. It’s also important to attach any necessary documentation to support the claim and ensure proper processing.
Avoiding Misuse of CO-45 Code
The CO-45 code should only be used for corrected claims, not for first-time submissions or those needing extra information or documents. Using it incorrectly can lead to claim denials or payment delays.
Impact of CO-45 Code on Medical Billing
The CO-45 code plays a key role in medical billing for healthcare providers. If a claim is denied because of this code, the provider won’t get paid for the service, leading to financial losses. A 2023 Medical Billing Trends Report found that incorrect use of adjustment codes accounts for 15% of payment denials.
To avoid this, it’s important to document and code all services correctly to reduce the risk of claim denials.
Identifying CO-45 Code Issues
Identifying the reason is the first step towards solving CO-45 code problems. This may include improper use of the code, errors in claim submission, denial, or payment delay.
Working with Medicare
After the problem is identified, providers can approach Medicare for assistance. This could mean contacting the Medicare Administrative Contractor (MAC) or Medicare Claims Processing Contractor (CPC) for advice and assistance.
Reviewing Claims
Providers are supposed to check their claims to confirm that they are submitted correctly and that the CO-45 in Medical Billing code is properly applied. This entails ensuring there is no error, verifying that all required HCPCS codes have been incorporated, and securing any documentation necessitated.
Correcting Errors
If errors or missing information are encountered, the providers should correct them and refile the claim using the CO-45 code. The refiled claim needs to be complete, accurate, and contain all supporting documentation needed to obtain approval.
How to Avoid CO-45 Code Errors?
In order to prevent CO-45 denials and avoid billing errors, healthcare professionals can take the following steps:
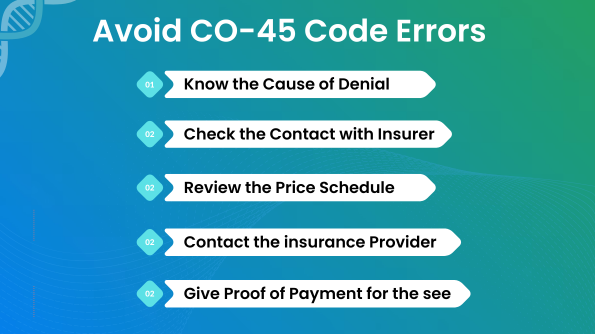
Read the Explanation of Benefits (EOB): Carefully read through the insurance provider’s EOB report to identify the reason behind the denial and the amount to be written off.
Check Your Contract: Make sure the amount billed complies with your contract with the insurance company and is not over the covered limit.
Compare Local Charges: If the billed amount is more than the insurance company’s maximum, check typical charges for the treatment in your locality to ensure your charges are customary and reasonable.
Request Reconsideration: If your charges fall within usual rates, call the insurer to dispute the denial and ask them to review the claim.
Supply Documentation: Send documentation of payment, like a fee schedule, invoice, or relevant medical reports, to underpin your claim.
Appeal if Necessary: If the claim continues to be denied, consider appealing or seeking dispute resolution services to challenge the decision.
By following these steps, healthcare providers can minimize denials and recover payments more effectively.
How to Appeal CO-45 in Medical Billing?
If you get a CO-45 denial code and feel it is unjust or incorrect, you can appeal. Check the status of the claim first to determine if the payment was posted to the patient’s deductible or coinsurance. If not, you can file an appeal with the insurance company along with supporting documentation.
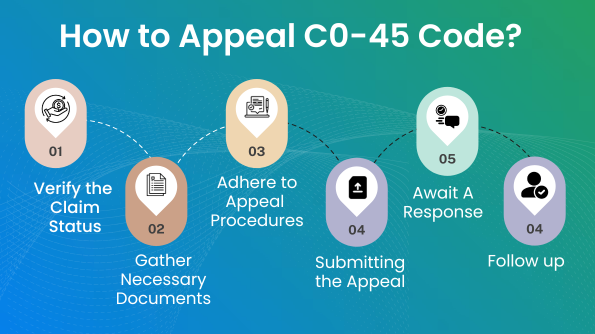
Attach a copy of the original claim, contract or policy information, a reason for why the denial is improper, and supporting documents like medical reports or billing information. Care must be taken to adhere to the insurance firm’s appeal processes and deadlines. Most insurers have an appeal within 120 days from the denial, and one can appeal online, by mail, or on the insurer’s official website.
Receiving a denial of CO-45 in Medical Billing is not the end of the process. If you think the denial was unfair, a well-documented appeal can make it more likely to have the claim approved.
Verify the Claim Status
Prior to proceeding, make sure that the payment was not credited to the patient‘s coinsurance or deductible. If it wasn‘t credited, you may proceed with the appeal.
Gather Necessary Documents
Original Claim
Keep a duplicate of the original claim, which was denied and has the CO-45 in Medical Billing.
Contractual Agreement
If you received the service under a particular contract with the insurance provider, have the contract available.
Reasoning for Appeal
Write a concise statement of why you think the denial was wrong.
Supporting Documentation
Collect any applicable paperwork, like medical records, referral letters, or lab tests, to support your case.
Adhere to the Insurance’s Appeal Procedures
- Find out how the insurance company processes appeals. Every insurer is different, so be sure to use their own guidelines.
- Be aware of deadlines. Most insurers provide up to 120 days to appeal, but it’s always best to check their precise time limit to avoid any complications.
Submitting the Appeal
Online
Most insurance companies have an online platform where you can submit an appeal. Ensure you have digital copies of all the required documents before you start.
Via Email
If the insurer accepts appeals through email, attach the documents and send them to the appropriate email address.
Tip: Always have proof of your submission, e.g., a screenshot, confirmation email, or any response from the insurer.
Await a Response
After you submit your appeal, the insurance company will consider it. This might take several weeks or several months, depending on their policies and the nature of your case.
Follow-up
If you do not hear back within the timeframe you expect, contact the insurer. Have all the details of your initial appeal at hand when contacting them.
Being transparent, well organized, and having the proper documentation is likely to improve your chances of getting the denial reversed.
Conclusion
Accuracy is critical in medical billing. CO-45 in Medical Billing is a key code to know, as it impacts reimbursement and can cause financial problems if not processed properly.
Understanding CO-45 is not merely about knowing its definition—it is also about knowing how it impacts healthcare services, patient access, and a provider’s financial stability.In order to avoid issues with CO-45 in Medical Billing, health care practitioners ought to exercise best practices, keep abreast of billing standards, and be properly documented. This ensures ease of operations, timely payments, and uninterrupted quality services without any monetary losses.
Handling CO-45 adjustments efficiently is crucial for optimizing the revenue cycle and maintaining compliance with payer agreements. At Keizer Technologies, we specialize in streamlining medical billing processes, helping healthcare providers navigate insurance adjustments like CO-45 while maximizing revenue and reducing denials.